|
Click HERE to Find Out How You Can Achieve Thyroid Levels within a Short Period of Time |
What
is Coeliac disease?
For
some people avoiding gluten is a very serious issue as their immune system
reacts abnormally to gluten.
Termed
coeliac disease, this digestive disorder is associated with inflammation and
damage to the lining of the small intestine. This then leads to a range of
health problems.
Coeliac
disease is one of the most common inflammatory conditions affecting the
digestive system. A gluten free diet is advocated for life for those diagnosed
with this digestive problem.
Individuals
with coeliac disease are so sensitive to gluten that they are not able to eat
any foods containing gluten as even a minute amount will prompt a swift immune
reaction.
The
prevalence of coeliac disease is increasing worldwide. It affects people of all
ages, both male and female. Until recent times it was considered a genetic
disorder that was discovered during childhood.
A
genetic predisposition for developing this problem does exist. However environmental
factors play a key role in triggering coeliac disease at any age. This
digestive problem can be set off by a stressful event, such as a major
infection, injury or surgery.
If
a person is unaware their poor health is due to Coeliac disease and they continue
to consume gluten containing foods the lining of the digestive system becomes
severely damaged. Over time, this leads to low intake of essential nutrients
and a further decline in health due to malnutrition.
Going
Against The Grain
These
days highly refined wheat is the most common source of gluten as it is used in
a wide variety of foods found in supermarkets. To meet ongoing demand wheat is
grown on an industrial scale.
Along
with the development of modern agricultural methods there has also been
selective breeding of wheat. Wheat crops now yield a much higher ratio of
gluten. The modern, hybrid wheat varieties may be contributing to the higher
prevalence of coeliac disease worldwide.
Dr.
William Davis is a respected cardiologist and author of ‘Wheat Belly: Lose
the Wheat, Lose the Weight, and Find Your Path Back To Health‘. He believes
aggressive breeding methods and genetic manipulation have turned wheat into a
‘Frankenwheat’.
Watch
these 2 videos on how to make the right food choices for naturally treating
coeliac disease
The
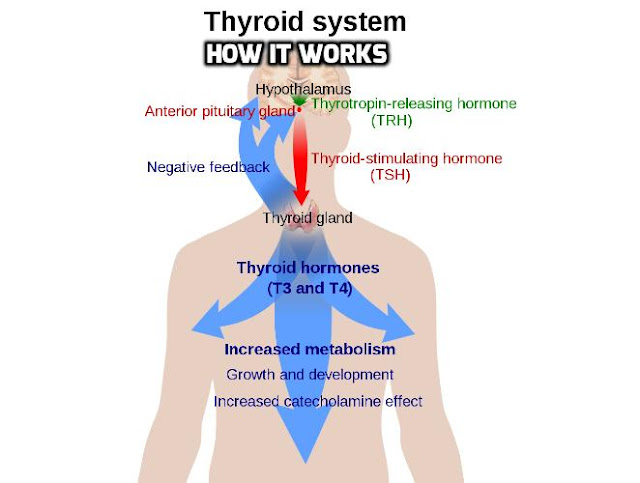
Selenium -Thyroid Connection
After
iodine selenium is the next most important mineral affecting thyroid function.
Several studies have shown that coeliac disease is associated with an increased
risk of developing an autoimmune thyroid disease. This is due to low selenium
intake or poor absorption of selenium.
The
thyroid is particularly sensitive to selenium deficiency because the selenium
dependent enzymes are vital to assist activity of the thyroid hormones,
including activation of T4 to T3.
Selenium
also plays a role in protecting the thyroid gland itself as this mineral boosts
glutathione activity. Glutathione is naturally produced by the body using
selenium and a combination of three amino acids sourced from dietary protein –
cysteine, glycine and glutamine. Glutathione acts as a potent antioxidant and
is highly active within the thyroid to help protect this important gland.
Long
term undiagnosed coeliac disease causes damage to the digestive system. This
leads to malabsorption of essential nutrients which over time is linked to poor
health due to malnutrition. A specific diagnostic test is used to confirm
coeliac disease.
The Natural Thyroid Diet
guidelines recommend excluding all gluten foods as part of a holistic strategy
to recover your thyroid health.
Watch
this Video
Read
the following related articles:
Author Bio:
Louise O’ Connor,
the author of The Natural Thyroid Diet –The 4-Week Plan to Living Well, Living Vibrantly, who
is a specialist in Thyroid Health. She is a highly regarded Australian
Naturopath and founder of Wellnesswork.
The Natural Thyroid
Diet goes beyond diet advice and offers practical and effective ways to achieve
healthy thyroid levels within just a short period of time. For more details,
Click on
The-Natural-Thyroid-Diet.com